This article is designed to give a simple overview of the subject of fascia and is not by any means a comprehensive treatise on the subject.
Fascia as a word is one which has only relatively recently become popularised, some would say inappropriately so, within the field of human anatomy.
Fascia is defined as a sheet or band of fibrous connective tissue enveloping, separating, or binding together muscles, organs, and other tissues of the body.
The important thing to remember about fascia is that it is one type of connective tissue in a family that has many members. All fascia is connective tissue, but NOT all connective tissue is fascia.
There are four types of connective tissue that can be categorised in the following manner.
Proper Connective Tissue,
Blood,
Bone,
Cartilage
There are some surprising facts surrounding connective tissue, apart from the fact that blood is and muscle isn’t. The most important fact of note is that connective tissue is made up mostly of non-living material known as the extra cellular matrix or ECM. This ECM is to some degree as, if not more important than the cells that are contained within it and make all movement and function possible.
ECM is like the inner ocean of our bodies. All the cells that we have require space around them and this space is filled with an inert fluid that protects, cushions and holds the cells and tissues in place. The ECM has several substances that allow for repair to take place, but the essential job of it is to facilitate the smooth actioning and function.
Not all ECM is the same and has different qualities depending on which type of cell produced it in what area of the body. Blood for instance has it’s own type of ECM which is plasma. It is the plasma that holds the red and white blood cells in place and carries them around the body. Blood is comprised of over 55% plasma and, like many connective tissues, is the forgotten yet vital component many systems.
Types of Fascia
The classification of fascia is not as straightforward as we might either hope for or believe. The layer of tissue lying directly underneath the skin is known as superficial fascia – SF and although predominantly comprised of adipose, is still a functioning fascial layer.
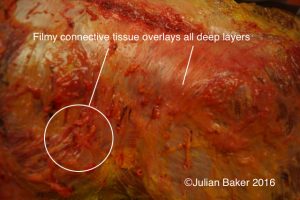
Irrespective of the amount of adipose laid down in the body, there is still a requirement for this to be held in place by a network of collagen based fibres as demonstrated by this dissection picture. This fibrous network allows for strength, movement, flexibility and adaptation to take place, as well as for variation in adipose distribution to be supported.

The deep layer of superficial fascia combined with adipose to form a single unit overlying the deep fascia and musculature of the gluteal region.
The superficial layer can often be removed in one whole unit, almost like a fleecey jumpsuit demonstrating that the tissue referred to as superficial fascia is a body wide structure, present virtually everywhere.
Even if someone were to lose almost all their adipose tissue, the fibrous network would still be in place, visible and palpable and attached to the skin by a transparent, filmy sheath. When you pinch your skin and lift it, anywhere in the body, you are picking up not just skin, but superficial fascia. The slippery, filmy layer between these tissues and the deep fascia is what holds it in place and stops if from getting pulled off completely.
Most people in the exercise world have complicated relationships with the layer we refer to as the superficial fascia. “Can you pinch an inch?” was the phrase that was used a few years ago to suggest that perhaps you were putting on too much weight or getting flabby.
In fact the SF plays a vital role in the stabilisation of our body and is home to some interesting material, in particular a hormone called leptin.
Leptin is a hormone which regulates the fat cells in humans and also is linked to appetite. When we eat we become full and it is this full feeling which is driven by Leptin. In obesity the levels of leptin drop, hence the feeling of being full is harder to come by. One of the reasons that the human has become a successful species, is our ability to keep taking in calories and be able to store them. Ideal in times when it was feast or famine, but not so great when we can get cheap 24 hour fast food.
Sugar is a particular demon as far as the ability to lay down a fatty layer. If we think of this tissue as another form of energy, it’s easy to see how if we take in a large source of energy like a chocolate bar, we will need to store it somewhere. The fatty layer is an enthusiastic repository for this energy which, if not burned off will simply be converted into fat cells and stored for use another time. If there is another time of course.
Filmy fascia. Not a thing
The layers of superficial fascia and deep fascia although appearing distinct, are not separate or even different in terms of their make up. When the superficial tissue is cut away, it leaves behind the shiny white surface that can be identified, supposedly as deep fascia. It also leaves behind a remnant, to which the excellent US dissector Gil Hedley assigned the name ‘filmy fascia.’ His assertion is that this is a separate and distinct layer or tissue that presumably performs a specific yet undetermined function. This is not the case. The fibres of the superficial fascia that encase and envelope the adipocytes, descend from the skin and weave their way thorough whatever thickness is required to house the fat cells. At a certain point the function of the fibres changes and accordingly their nature does as well.
They become more dense, more tightly arranged and get assigned the term, dense fibrous connective tissue. They are still the same nature of the fibres that surrounded the fat cells, but have simply adapted to what is required of them. The nature of connectivity requires tension and some degree of continuity and these fibres descending towards the deep fascia and from their muscle, are no different. Once the connection has been cut, there no longer remains the tension and density of the tissues that were there and they fall, like a sheet of water stopped in mid air, upon the surface of the deep fascia.
To the naked eye it does appear that there is some kind of varied tissue existing that stands between the superficial and deep layers of connective tissue, but this is only there once the separation of these tissues has been created by the dissectors knife and simply don’t exist without it. The process of dissection is, by its very nature creative. It creates sections, layers, structures, and material that by their very nature are not separate and which have no independent purpose, except to be part of a greater whole. It is tempting to see things that appear under our scalpel as being inherently real, but this is just a mirage.
It’s similar to the way that we see a chicken drumstick or a pork chop as an item in our shopping trolley or on our plate, but fail to consider the feathers or the trotters. We rename things to suit our agenda or focus and whilst this is understandable, it can also be misleading if we don’t occasionally take the wider view in to account.
The layers of the body that we create in dissection are not actual layers as such. We call them layers and label them in order to be able to study them and understand more about what they do. In essence every part of the body is the same functional unit and certain tissues will be more solid and stable and others will be slippery and gliding, acting as smooth interfaces between tissues. The filmy layer that Gil refers to will have properties, but only where they are associated with the tissues above, below or around them. It is humans that have created the layers and who have then subsequently named them and studied them. Whilst there is no easy way around this process with the human brain as relatively clumsy as it is, it’s important to remember that these tissues, whilst interesting, are pointless unless subsequently incorporated into the bigger picture.
Deep Fascia
The connective tissue we call deep fascia has a different look, but in essence is still a form of connective tissue. All fascia is made up mostly of collagen, one of the most common proteins in the body. We make collagen every day of our lives and use it both to repair our connective tissue as well as create the connections and links from one part of the system to the other.
Nature hates straight lines and it is left to human endeavour to create firm, stable structures by piling things one on top of the other, such as bricks. In the natural world virtually everything, from the huge to the microscopic, is curved. Curved structures not only allow for tension to be absorbed, but also distributed and transmitted.
Even huge, stable structures like trees are made of curved elements that will allow sway and movement to occur in strong winds and changing conditions. The human structure is no different. A collagen fibre is a spiralled, triple helix that doesn’t form straight lines, but instead creates multi-directional layers that allow movement in lots of different directions.
It is also very adaptable and will lay down more fibres in a new direction of strain, if the movement and loading is repeated often enough. Collagen fibres are also responsible for repairing damaged tissue, when inflammation from injury acts as a signal for the system to produce more cells.
Not all collagen fibres will be the same in terms of density, direction or other composition and much is dependent on the function of the individual.

There are many different types of collagen but the two main types in the human body are types 1 & 3, with type 1 making up about 90% of our collagen fibres.
Tensegrity
One principle of understanding load mechanisms in the human form, is known as bio-tensegrity a term popularised by Steven Levin. The principle derives from the works made famous by a sculptor Kenneth Snelson, who designed tensegrity structures where solid pieces would appear to ‘float’. held in equal tension by the cords attached to them.
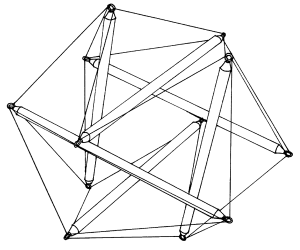
A tensegrity structure made popular by the sculptor Kenneth Snelson and used by many to explain how the body might work.
In much the same way it suggests the bones of the human float in a tensional sea of connective tissue, powered by muscle and held in place by skin. It’s a clunky metaphor as the relationships are a whole lot more complicated than some wooden dowels, but the imagery is captivating.
The nature of connective tissue is that it maintains separation as much as it creates connection. There are spaces all over the body that rely on being spaces in order for the human form to function effectively. The knee for instance will quickly break down when the space between the bones becomes reduced. Similarly spaces in the lungs allow for movement to take place and for fluid to be circulated. It’s the spaces that permit forces and tension to be absorbed as well as transmitted. The key element to keep remembering, is that in the human, these spaces are always filled with fluid.
Collagen lay down is not selective and will lay down according to the instructions we give it. In the following picture the fuzzy, cobweb like structures that lie between the muscle fibres are the naturally occurring collagenous fibres that need to be there in order for normal function to take place.
In a living body these would be wet and slippery and would create the framework for muscle to move around bone and force transmission to exist.
Muscle is the power house for movement. With no muscle, the ability to lift an arm or a leg would be limited. Without fascia it would be impossible.
Because the fascial system is continuous, it doesn’t stop at the bone when the muscle does, but carries on across planes and in different directions, allowing what some people feel is a communicating tensional network throughout the body.
In certain areas where the connective tissue is categorised as dense and regular, the sheets of deep fascia that we see, are criss crossed and formed from fibres that travel in multiple directions.
Each muscle is surrounded both by multi-directional sheets of fascia, but also has fascial fibres running through and around each compartment and every muscle fibre. The integrity of muscle relies entirely on the fascia that surrounds it and holds it in place.
If fascia facilitates muscular movement, it also has the capacity to respond to lack of movement as well. As already discussed, the essential ingredient in all connective tissues is fluid in the form of ECM. Within this fluid environment live the cells that produce the collagen, fibroblasts. These cells are responding to the information given to them in order to establish what is required.
Movement, pressure, loading and friction are all elements that will maintain the environment of the ECM. Without movement, the chances are that stiffness and thereby lack of fluid flow will result. The outcome is the stiffness that most of us will have experienced at some stage or the other but which if left to continue will get worse.
An extreme example is that of Amar Bharati a sadhu, who over 40 years ago decided to raise his arm above his head as a tribute to Shiva.
Over the years the pain that he first experienced, subsided to numbness. The collagen fibres surrounding the muscle tissue and the joint will, most probably, have become fibrous and hard. The effort of holding the arm up will have ceased to be an effort, with the fibres taking over the task of holding the arm in that position.
The rest of him keeps doing a good job. We can see him squatting on the ground demonstrating great flexion ability through his knees, hips and ankles. It’s a perfect demonstration of how continued movement leads to continued ability to move and how stillness leads to stiffness.
Movement between tissues is always going to be more limited than we think. A muscle is held in place firmly by the fascia that surrounds it. Other factors come in to play as well. An arm for instance contains nerves that extend from the neck down to the wrist. These nerve pathways are held in place in a strictly controlled environment and have no ability or need to be able to move around in hundreds of directions. To do so would be disastrous.
Similarly, muscles slide in a relatively limited plane of movement, again held firmly in place by filmy fascia and nerve pathways. The need for movement in the human form doesn’t need to rely on a model of extremes.
The treatment and stretching of fascia has attracted intense interest from the health and fitness industry over the last few years, with a myriad of ‘solutions’ to ‘release’ fascia that is tight, unhealthy, knotted, twisted: the list is extensive. The probability of this is that any movement, stretching or treatment doesn’t affect the fascia in that moment at all, but instead contributes to a healthier status over time.
Fascia can’t be stretched in the way that a jumper can. In order to elongate tissues such as fascia, sustained pressure and lots of time are needed. The pressure however is probably less than originally thought as even gentle movement and tension, applied over a long period, will have the mechanotransduction effect already mentioned.
It was always believed that stretching was a requirement for function and that stretching the fascia was what was happening as part of deep static movements. The evidence now suggests that in fact stretching, whilst assisting in general functional movement, is not required at all as a general rule. In many instances where chronic pain is present, the advice is often to stop stretching completely in order to allow function to be restored.
Neither can fascia be released in the way it is often suggested by myriads of therapies, labelled fascial release. It probably doesn’t need to be released in the first place as it’s unlikely that the pain being caused by any issue is coming solely from the fascia. Whilst fascia is full of nerve endings and touch receptors, pain, like movement, is a body wide mechanism.
What fascia does need is maintenance. Daily regular movement through a wide range without extensive stretching is likely to maintain the health and flexibility of fascia well into old age. The enemy of fascia is extended bouts of stillness.
Treatment is another issue where little or no agreement has been achieved. The fascia researchers tend to come from a field where a large amount of pressure is used to achieve change, whereas the suggestion now emerging is that less pressure applied more often might have better results.
The science of fascia is still new and there is much more work to be done before we can establish behaviours or patterns of fascial change beyond doubt.
What is conclusive is that the watery extra cellular matrix, surrounding and hydrating all our tissues, needs circulation that can only come from movement.
Whatever movement means to you, keep doing it.